Bringing the Rural Health Crisis Into Focus: Documentary Spotlights Dire Effects of America’s Healthcare Deserts
As hospital closures increase in rural America, it’s critical that everyone – from patients and community members to providers, health plans, local business leaders and legislators – understand the devastating impact that ripples across the areas affected. While it didn’t ultimately receive an Oscar nomination, we are thrilled to know one documentary short film in particular almost made it as a finalist for this year’s Academy Awards.
It’s called If Dreams Were Lightning: Rural Healthcare Crisis, and it’s a poignant piece casting a much-needed spotlight on the “healthcare deserts” of America’s small towns. It opens with the true story of an abandoned community hospital sitting empty. Once the center of health and life – where babies were born, injuries were healed and lives were saved – the building itself is now used by paranormal researchers who want to connect with ghosts.
From there, the 25-minute film (which you can scroll down to watch below) follows the tragic stories of patients and families up and down the rural byways of the impoverished Appalachian region. The journey is as real as it is heart-wrenching. And for those reasons, it must be seen and heard.
“Rural hospital closures, decreasing reimbursements, declining operating margins, and staffing shortages have all coalesced to undermine the delivery of care in communities whose populations are older, less healthy, and less affluent. The mission of the safety net to serve under-resourced communities is unraveling.”
— Chartis Center for Rural Health
Why This Message Matters
Rural hospitals make up about one-third of all hospitals in the U.S. – and among them, roughly a quarter (23 percent) are now at risk of closing. A full 50 percent of rural hospitals are currently operating in the red (which is up from 43 percent just 12 months ago). Operating at losses leads to bleak outlooks. That community-hospital-turned-ghost-hunter-haven that was featured in the documentary? Before it had no choice but to shutter its doors, the hospital was offered to Veterans Affairs (the VA) to buy for a single dollar, and the VA declined.
Nearly 20 percent of U.S. residents – over 66 million people – live in rural America. Many depend on their local community hospitals as the only sources of care they can get to. They are essential safety nets – not to mention major employers – for rural residents across the country. And yet, according to recent findings from the Chartis Center for Rural Health:
- In the last 14 years, 167 rural hospitals have either closed completely or converted to outpatient care only.
- Between 2011 and 2021, 267 rural hospitals shuttered their OB services – which represents a loss of nearly 25 percent of America’s rural OB units.
- Between 2014 and 2022, 382 rural hospitals have stopped providing chemotherapy services.
- Critical access hospitals are seeing reimbursement rates plummet as Medicare Advantage (MA) now accounts for 35 percent of all Medicare-eligible patients in rural communities. In some states, it now exceeds 50 percent.
For these reasons and many others, If Dreams Were Lightning is perhaps the most relevant film you won’t hear mentioned in the Short Subject Documentary category at this year’s Oscars. But fortunately, the publicity and attention that came with being shortlisted for an Oscar helped bring awareness to the director Ramin Bahrani’s cause. The film has been screened at several festivals and is available to watch from PBS – click below to watch it now:
At Dobies Health Marketing, we are sharing this film because we are passionate about contributing to a world where rural healthcare can thrive, not merely survive. Through our rural health division (dhmstudio+), we bring decades of experience to rural hospitals, delivering affordable, effective, strategy-first marketing solutions that make their organizations stronger and more sustainable. From building the value of primary care to building community partnerships for health, we are committed to advancing rural health in communities across the country. If you are part of a rural hospital team and want to hear more about the work we do to support rural health, contact us today.

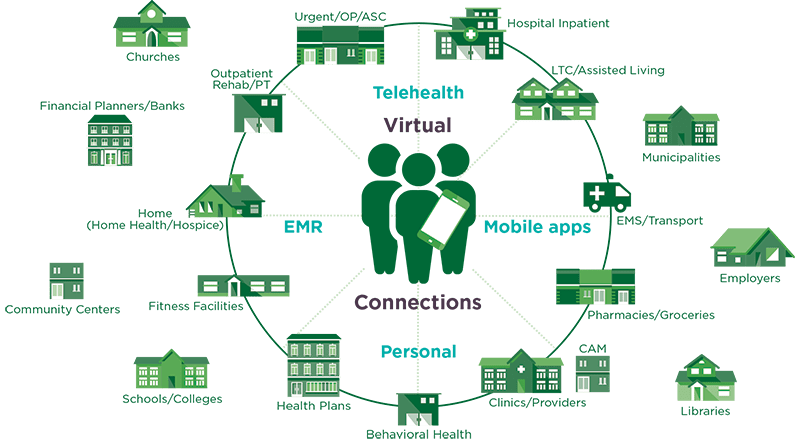
 For rural hospitals and healthcare providers, understanding patients – who they are and how they interact with you, each other and your larger urban center competitors – is an important aspect of patient experience and marketing strategy.
For rural hospitals and healthcare providers, understanding patients – who they are and how they interact with you, each other and your larger urban center competitors – is an important aspect of patient experience and marketing strategy. October is National Health Literacy Month – an important reminder to reflect on our roles in helping every patient and consumer understand the health options before them. Whether you provide care or promote those who do, communicating in ways that are clear for everyone can make a very healthy difference.
October is National Health Literacy Month – an important reminder to reflect on our roles in helping every patient and consumer understand the health options before them. Whether you provide care or promote those who do, communicating in ways that are clear for everyone can make a very healthy difference.
 Over the last few weeks, we have been discussing
Over the last few weeks, we have been discussing 
 As we continue our series on
As we continue our series on 
 KANSAS CITY, Mo. – Dobies Health Marketing, a strategy-first healthcare marketing firm, has launched
KANSAS CITY, Mo. – Dobies Health Marketing, a strategy-first healthcare marketing firm, has launched 